The voicemail seems ordinary at first: a message from your CFO asking finance to "push through a vendor payment before audit deadlines." The tone, cadence, and urgency all feel right. But the call isn't from your CFO. It's a deepfake engineered from public audio clips and sent during shift changes, when response times are naturally stretched thin.
Attacks like this are escalating across the healthcare sector. According to the 2025 Verizon Data Breach Investigations Report, nearly three-quarters of healthcare breaches fall into patterns driven by human decisions or operational missteps, including system intrusion, miscellaneous errors, and behavior-driven "everything else" incidents.
For security leaders, these trends point to a clear operational gap. Traditional, generic training doesn't reflect the pace or complexity of healthcare environments. Clinical teams operate under time-sensitive patient demands, and administrative staff handle high volumes of sensitive data.
Modern threats, from vishing and smishing to AI-generated impersonation, require training grounded in real workflows, not theoretical best practices. This guide will help you close that gap.
We'll cover role-based training guidance, practical implementation steps that fit healthcare operations, and clear KPIs rooted in behavioral risk, so you can strengthen human defenses without disrupting patient care.
Why healthcare needs role-specific security training
Healthcare environments give social engineers exactly what they need: urgency, constant interruptions, and heavy reliance on email and phone communication.
It's no surprise that 60% of healthcare IT leaders report at least one email-related security incident in the past year, underscoring how human-driven risk now defines the sector's threat surface.
In this context, HIPAA compliance isn't enough. Regulatory safeguards don't prepare staff for real-world tactics like vishing, smishing, or deepfake impersonation—attacks designed to exploit trust and pressure, not technical gaps.
Different teams also face fundamentally different cyber risks.
- Front desk staff manage identity verification and high-volume communications.
- Clinicians make rapid decisions in time-sensitive environments.
- Administrative and IT teams handle financial data and access controls targeted by impersonation attempts.
When the stakes include patient safety and operational uptime, one-size-fits-all training simply doesn't work. Healthcare organizations need role-specific guidance that reflects actual workflows and equips every team member to recognize and respond to modern social engineering threats.
Designing a modern security awareness training program for healthcare
A modern healthcare security program starts with understanding human risk, not just technical exposure. Leaders need clarity on where behavior-based vulnerabilities exist across clinical, administrative, and support teams. Mapping those risks provides the foundation for a program that strengthens real decision-making, not just compliance posture.
From there, you must tailor content to job functions and learning styles. Healthcare teams operate under time pressure, so high-impact training—short, contextual, and workflow-aware—drives far better retention than long-form, generic modules.
Brief onboarding content, quarterly refreshers, and just-in-time nudges ensure that security isn't a one-and-done requirement but an integrated part of everyday operations.
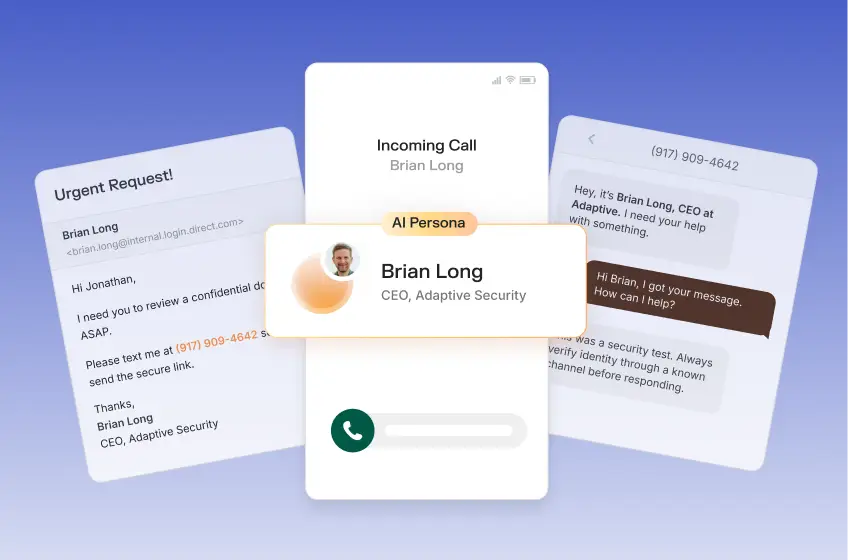
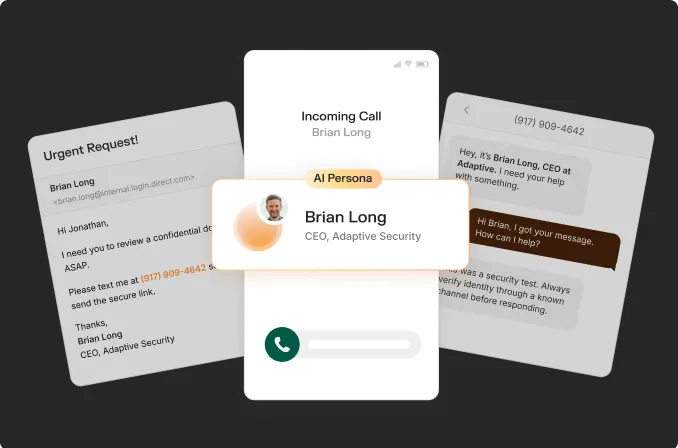
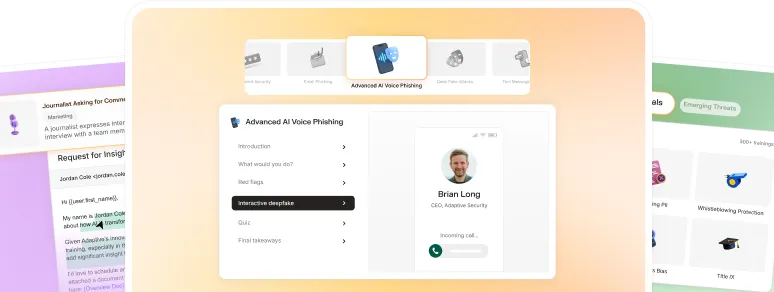
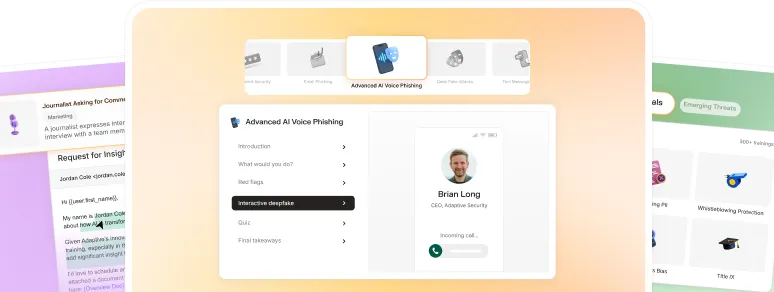
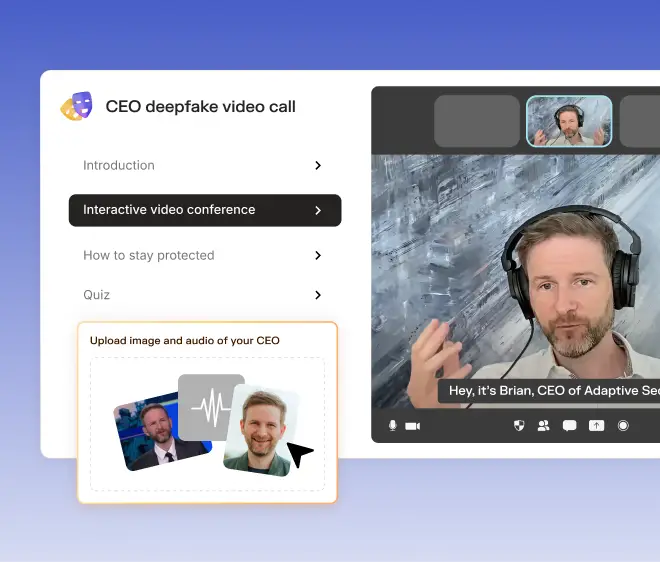
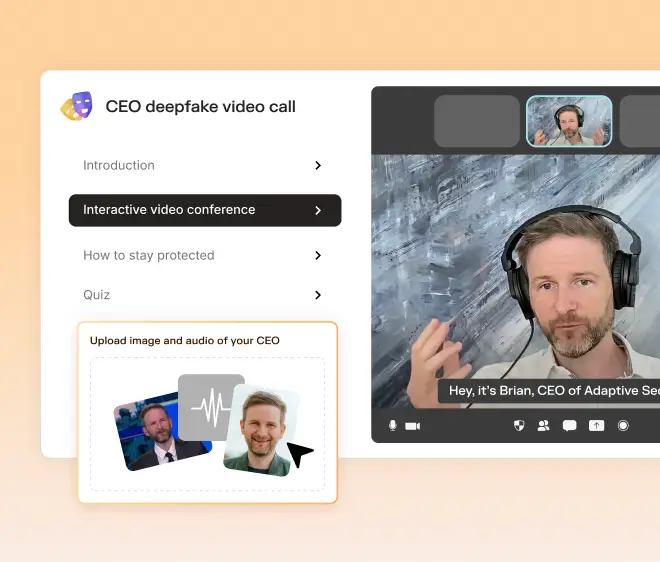
This is also where simulation design matters. Modern cybersecurity threats increasingly involve deepfake impersonation, smishing, and targeted spear phishing, and simulations need to reflect that sophistication. Many healthcare providers are already shifting to AI-native training models.
At Mt. San Rafael Hospital, staff engagement increased significantly when the training program included a deepfake video using the CIO's voice—making the threat feel real and personal without creating fear or blame. That's the impact of simulations built around actual workflows and real hacker tactics.

(Source)
For healthcare organizations, the goal isn't simply to "deliver training"—it's to build a workforce that can recognize and respond to modern attacks under real conditions. That requires programs shaped by human risk insights, aligned to the way each team actually works, and flexible enough to adapt as new threat patterns emerge.
Implementation checklist: Step-by-step for healthcare teams
A strong security awareness program succeeds when it's rolled out with the same discipline as any other clinical or operational initiative. These steps help healthcare teams implement security awareness training platforms in a practical, measurable way.
Step 1: Secure leadership buy-in and assign a program owner
Effective cybersecurity readiness starts with clear ownership. Designate a program owner, often within Security, Compliance, or HR, to align expectations, set timelines, and manage rollout across departments.
KPIs:
- Executive participation rate in kickoff briefings
- Completion of an annual cybersecurity training roadmap
Common pitfall: Treating training as an IT-only responsibility, which leads to inconsistent adoption across clinical and administrative teams.
Step 2: Segment employees by risk profile
Use a risk assessment to segment employees into groups such as clinical staff, front desk teams, administrative functions, and IT. Each group encounters different cyber threats, and segmentation ensures the program reflects those realities.
KPIs:
- Completion of risk segmentation across every department
- Percent of employees assigned to a role-appropriate training track
Common pitfall: Relying on job titles alone—risk profiles should reflect access levels, workflow pressures, and real communication patterns.
Step 3: Map content to real-world threat scenarios
Connect security awareness training topics to attacks healthcare teams actually face, such as HIPAA-related data leaks, impersonation attempts, smishing targeting patient scheduling lines, or deepfake escalation scams. This ensures teams can spot cyberattacks that mirror their daily workflows.
KPIs:
- Number of role-specific modules or simulations deployed
- Reduction in repeat failures on the same scenario type
Common pitfall: Overloading staff with generic content that feels disconnected from clinical or operational realities.
Step 4: Launch with a kickoff and first simulation
Introduce the program with a brief kickoff that explains expectations, timelines, and why the organization is prioritizing modern security awareness training. Then deploy a baseline simulation to capture initial behavioral risk data.
KPIs:
- Kickoff attendance or acknowledgment rate
- Baseline simulation completion and failure rates
Common pitfall: Launching simulations without context, which can create confusion or reduce trust.
Step 5: Measure, report, and iterate quarterly
Quarterly reviews ensure the program stays aligned with evolving threats and organizational changes. Track performance trends, identify high-risk segments, and update content where behavior isn't improving.
KPIs:
- Quarterly reduction in risky actions (such as clicks, replies, credential entries)
- Improvement in departmental completion and engagement rates
Common pitfall: Reporting on compliance only; leaders should track behavior change, not just training completion.
What to train: Threats healthcare professionals actually face
Healthcare teams interact with patients, families, vendors, and internal staff across phone, email, text, and even social media. This creates a broad attack surface that traditional training rarely covers. A modern program needs to prepare employees for the specific tactics attackers use to infiltrate clinical and administrative workflows.
The following threats represent the scenarios most frequently exploited in healthcare environments:
- Deepfake voicemails or videos impersonating surgeons, finance leaders, or on-call administrators to request urgent approvals, transfers, or access changes.
- Smishing attempts targeting patient-facing staff, often disguised as scheduling updates, insurance questions, or pharmacy requests.
- QR code phishing left in waiting rooms or hallways, directing patients or staff to malicious portals that capture credentials or download malware.
- Social engineering near nurses' stations, including portable device theft, badge tailgating, and impersonation of new clinical staff or technicians.
- Social media manipulation, where attackers pose as family members, vendors, or job seekers to build trust and extract sensitive information.

(Source)
Adaptive Security's security awareness training helps teams prepare for these scenarios with simulations that mirror real healthcare interactions. By training against the threats employees truly encounter, organizations strengthen both compliance and day-to-day readiness.
Healthcare organizations such as Xenon Health cite Adaptive's AI-driven features, strong phishing simulations, and ease of use as critical to keeping staff ready for evolving threats.
How to measure program effectiveness in healthcare
A security awareness program only delivers value when leaders can track measurable behavior change, not just training completions. Healthcare teams need KPIs that show whether staff can recognize, report, and respond to real-world threats without slowing down patient care.
Core KPIs to track:
- Simulation click rate and repeated clickers to identify high-risk users who need targeted retraining.
- Role-based risk scores that compare performance across clinical, administrative, HR, and IT teams.
- Retraining completion and improvement rates following failed scenarios.
Compliance and audit-readiness metrics:
- HIPAA-mandated training adherence, including modality, frequency, and documentation.
- Audit-readiness indicators, such as evidence of ongoing training, role-specific content, and incident-response education.
Behavioral leadership metrics:
- Time-to-report suspicious messages, a leading indicator of real-world readiness.
- Volume and quality of security incident reports, showing whether staff feel confident escalating concerns.
Adaptive Security provides healthcare organizations with dashboards that visualize these metrics by department, function, and risk segment. This makes it easier to monitor progress, demonstrate compliance, and prioritize intervention.

(Source)
Healthcare teams like Shasta Community Health Center have seen the impact of this visibility firsthand. By adopting Adaptive's AI-powered phishing and deepfake simulations, Shasta gained clear, department-level insight into which roles faced the highest risk.
They then used that data to deploy targeted, HIPAA-aligned training that significantly improved employee readiness. Their experience underscores a simple point: data-driven visibility is what turns security training into meaningful risk reduction.
Why purpose-built tools matter for healthcare security awareness
Healthcare operates in an environment where human error can have clinical, financial, and regulatory consequences. Fast-paced roles, constant interruptions, and complex data flows create risks that generic security training simply can't address.
Modern threats like deepfakes, smishing, impersonation scams, and targeted social engineering require simulations grounded in the reality of clinical and administrative workflows.
The most effective programs focus on behavior, not checkboxes. They're measurable, adaptable, and engaging enough to help staff recognize and respond to threats under real conditions. Purpose-built platforms make that possible by aligning security training with how healthcare teams actually work.
Train your clinical and administrative teams on real-world threats, from deepfakes to smishing. Book a custom demo with Adaptive Security today.
FAQs about healthcare security awareness training
What makes healthcare uniquely vulnerable to security threats?
Healthcare is uniquely vulnerable because constant urgency, sensitive data, and fragmented workflows create ideal conditions for social engineering and impersonation attacks.
What are the most common human risk scenarios in healthcare?
The most common scenarios include phishing, smishing, deepfake impersonation, misdirected emails, and rushed access decisions at nurses' stations or front desks.
What's the ideal frequency for security awareness training in healthcare?
The ideal approach is to deliver short onboarding training, quarterly refreshers, and just-in-time nudges supported by ongoing phishing simulations.
How do you tailor security training for clinical vs. administrative staff?
Training for clinical staff should focus on fast, scenario-based content aligned to patient workflows, while administrative teams need modules on financial requests, data handling, and escalation protocols.
Can security awareness training help with HIPAA audits?
Yes. Role-specific training, documented completion, and behavioral metrics directly support HIPAA audit readiness and demonstrate continuous compliance.


As experts in cybersecurity insights and AI threat analysis, the Adaptive Security Team is sharing its expertise with organizations.
Contents